Dr. Jessi Gold is the Chief Wellness Officer of the University of Tennessee System and an Associate Professor of Psychiatry at the University of Tennessee Health Science Center, where she primarily sees healthcare workers, college students, and trainees.
What’s the big idea?
Doctors aren’t feeling well. With toxic work culture afflicting all industries, the medical profession has found itself hit particularly hard by the normalization of burnout. How Do You Feel? offers burnout advice for maintaining wellbeing as a healthcare worker, and as a society.
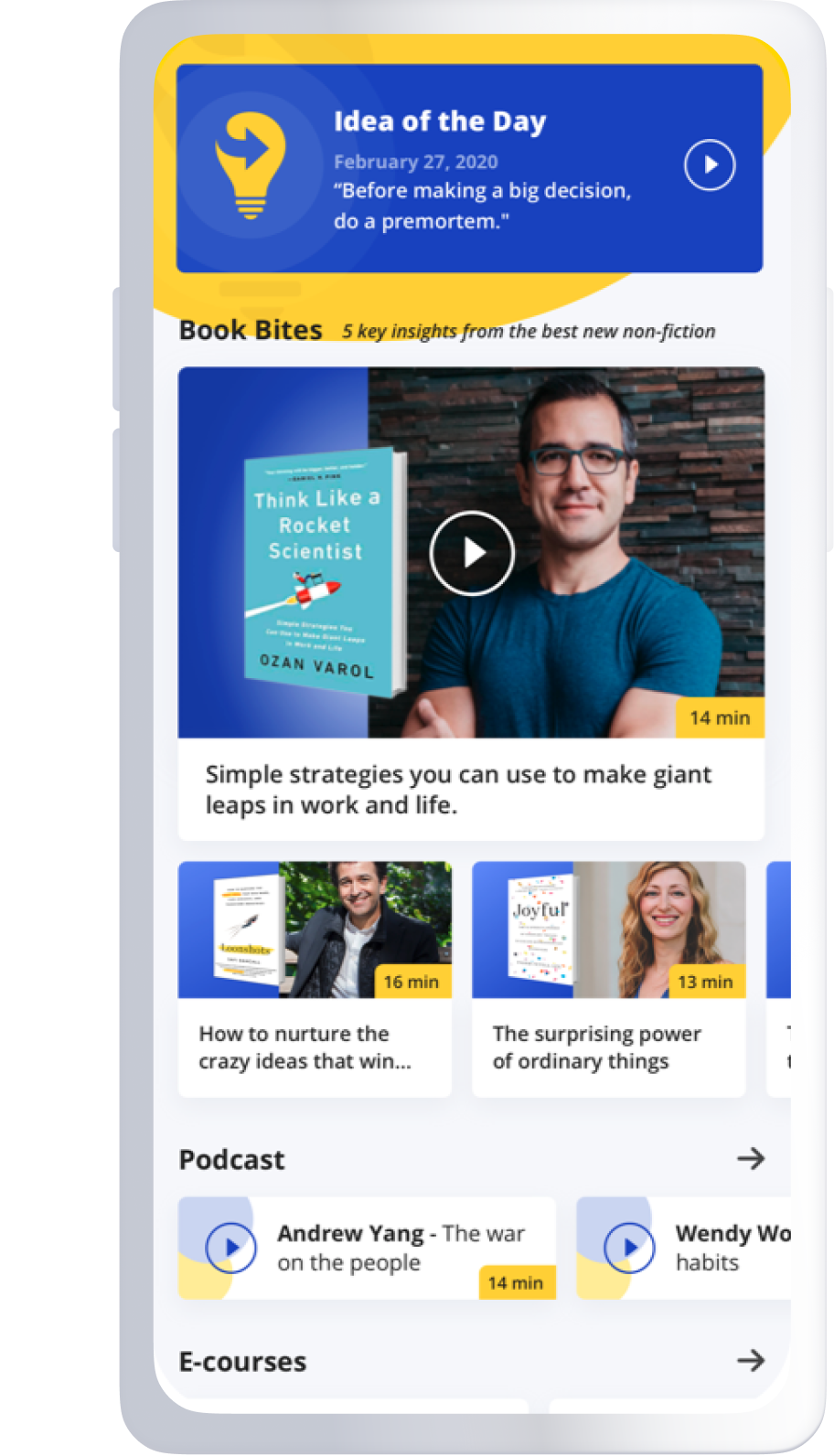
Below, Jessi shares five key insights from her new book, How Do You Feel?: One Doctor’s Search for Humanity in Medicine. Listen to the audio version—read by Jessi herself—in the Next Big Idea App.

1. We are not just OK or fine.
In casual conversation, have you ever noticed how often you ask someone how they are doing or feeling, and most of us just pause and answer by saying OK or fine—which aren’t actually feelings? In psychiatry, we say FINE means Feelings I’m Not Expressing. The desire to say OK or fine is because we don’t have authentic conversations on these topics and are afraid to be vulnerable. We also don’t want to admit the truth to others (or even ourselves) when we are not fine.
This is particularly true among healthcare workers. Long before COVID, we had burnout rates as high as 50 percent. Burned-out physicians have lower patient satisfaction and more errors. They also leave the profession. COVID compounded this, and CDC data shows that burnout and intent to leave both increased. We need to care about those who care for us. That group, too, needs to feel that it’s OK to focus on themselves. It isn’t selfish. It’s necessary.
2. Identifying your own burnout is hard because it goes beyond work.
We use the term “burnout” colloquially to mean “work was hard,” but it really means our workplace made us feel emotionally exhausted, depersonalized, and have a reduced sense of personal accomplishment. These things look different in different people, but for the most part, many of us think those symptoms are the products of work for everyone.
I often hear things from patients like, “Of course, I’m emotionally exhausted—I listened to patients’ traumas for hours.” Or, “Of course, I am getting less done; this week was just busy.” We also learn to minimize burnout because it is normalized. We look at the others in our workplace and notice they are also not sleeping or functioning. So, we suppose that this is how work is supposed to feel. One study asked surgeons in the bottom 30 percent of a validated measure of well-being how they thought they did, and most thought they were average or above average. Surgeons are a particular subculture, but I think we’d see similar results in other fields.
“We blow off early warning signs, like a subtle change in our schedule or overwhelm, and wait until we fall asleep every day after work without knowing why.”
When we look next to us and see that a coworker is sleeping less than I am or functioning equivalently badly, we assume we’re good. As a result, we blow off early warning signs, like a subtle change in our schedule or overwhelm, and wait until we fall asleep every day after work without knowing why. Even when I reached that point, I still didn’t call it burnout. If it is hard for me, a burnout expert, to identify it in myself, then it is for most.
3. Asking yourself how you’re feeling can make a big difference.
One way to intervene against burnout or ask for help earlier is by purposefully checking in on ourselves, asking, how do I feel? It seems simple, but most of us never do it because we spend so much time asking others how they are, that we forget about ourselves. Honestly, when my therapist asked me if I had ever asked myself that question, I realized the answer was no. Maybe it was because medical school taught me to ignore my own hunger or need to go to the bathroom. Or because my supervisors modeled to me that showing up at work sick (even if I needed to drag my own IV pole with fluids) was cool and the only acceptable option.
Knowing your own early symptoms (for me it’s anger over email) can help you know when you are inching toward burnout, and let you practice self-care or a coping skill. Maybe it’s mindfulness, or maybe you hate mindfulness, but whatever you do, you can make a choice that might help counter these subtle changes. If you wait until you are 10/10 burned out, time off is all that will help.
4. Combat perfectionism with compassionate self-talk.
Our culture tells us we shouldn’t have feelings, that successful people somehow don’t, and that having them at all is a weakness or failure, which collides with the fact that so many of us are perfectionists.
We seem to believe that if we are good at our jobs, we should not make mistakes or fail. This expectation, especially in the setting of challenging or unrealistic goals, is maladaptive. If failure is not seen as an option, the impact of failure is much greater and can lead to feelings of inadequacy, depression, anxiety, and burnout.
“We can pause and reframe our response to how we would talk to a friend.”
Take doctors as one example. One study looks at how they view their mistakes: do they see them as self-condemnation and their own fault, or self-encouragement and an experience to learn from? The study found their rates of self-condemnation were about 50 percent higher than workers in other fields. When the researchers controlled for that difference in perception, the significant difference in burnout between physicians and other professions was no longer seen. This doesn’t mean that burnout is only a result of this mindset, but it does mean that understanding perfectionism and how we view mistakes can help us combat it.
We can do that by practicing self-compassion. If we make a mistake when the voice in our head says, you’re an idiot, or you’re horrible, instead of believing it, we can pause and reframe our response to how we would talk to a friend. To that friend, we’d have more balanced thoughts like, “It’s ok; you tried your best and were not perfect; none of us are.” If we start catching our automatic thoughts over time, we will learn to be kinder to ourselves, which can help our self-esteem and prevent burnout. Sometimes, little things make a big impact.
5. Sharing our stories can change culture.
Many of us struggle in silence. Normalizing burnout starts with talking about it. Vulnerability isn’t easy, but it is a superpower. It is how we will change work cultures for the better.
Not everyone has to say they have been burned out or, like me, take psychiatric medication (though it is nice if some people do). We just need to start saying some of the challenges and quiet parts out loud: work/life balance is hard, witnessing codes is emotionally traumatic, I didn’t really sleep last night, etc. Those simple statements can make us feel supported and less alone. They will also make it easier for us to ask for help when we need it and feel less shame and guilt when doing so. So, really, truly, how do you feel?
To listen to the audio version read by author Jessi Gold, download the Next Big Idea App today: